-
article · 2025Year39Moon18Day
Flex 工作站在蛋白质定量实验中如何操作更高效?
Read More -
article · 2025Year8Moon17Day
Opentrons Flex 使用中常见问题有哪些?
Read More -
article · 2025Year5Moon16Day
如何通过 Flex 提高蛋白质组学实验产能?
Read More
As COVID-19 spreads rapidly, global health systems are increasingly overwhelmed by the number of people requiring diagnosis, isolation, and treatment. There are glaring deficiencies in everything from staffing and fast and reliable testing facilities to the availability of hospital beds and critical medical-grade equipment. The scale and breadth of the problem requires an equally substantive response not only from frontline workers such as medical personnel and scientists, but also from a skilled public with the time, facilities and knowledge to contribute meaningfully to facilitate a comprehensive global response. Here, we summarize community-driven approaches based on free and open source scientific and medical hardware (FOSH) and personal protective equipment (PPE) that are currently being developed and deployed to support the global response to COVID-19 prevention, patient treatment, and diagnostics response. Release date: April 24, 2020
Introduction In recent days and weeks, governments around the world have called on industry to address key shortcomings in the global response to the coronavirus pandemic, such as producing more personal protective equipment (PPE), ventilators and diagnostic tools [ 1 , 2 ]. While this is an important component of any country’s response to an epidemic, existing industry capabilities may be insufficient to address this challenge [ 3 – 5 ]. Furthermore, this approach would first address shortages in the regions where the relevant industries are located, rather than global shortages, and at a time when the economy is being hit hard, the medical-grade equipment and kits produced through this process will be expensive. Clearly, product innovation and novel manufacturing processes are essential.
Here, a complementary avenue for acquiring much-needed tools and equipment is Free and Open Source (Scientific and Healthcare) Hardware (FOSH). FOSH follows the ethos of open source software, where all blueprints of tools are freely available under appropriate licenses so that anyone can study, learn, modify, customize, and commercialize them [ 6 , 7 ]. Research and practical experience on FOSH show its key advantage that is crucial in disaster situations: rapid and distributed development based on the contributions of many people, most of whom work remotely [8, 9]. This is highly advantageous considering the social distancing measures implemented in many countries affected by COVID-19. FOSH is typically much cheaper to implement [ 10 ] and is easily adaptable to local resources, which is another key advantage of the open hardware approach.
Finally, and perhaps most importantly, any new hardware design or improvement is by definition globally available. Anyone with the necessary knowledge, tools, and time can use this knowledge to provide meaningful support to their community. The importance of the latter cannot be overstated: different communities face different constraints on the availability of trained staff, medical supplies and machines, and diagnostic tools. As a result, restrictions in one place may not apply in another, so any global response must be tailored to local realities. Here, the many benefits of the FOSH approach enable rapid local deployment, thereby bypassing traditional production chains and providing flexibility to supply affected areas as they arise. While this is useful worldwide, it may be particularly important in areas that have traditionally had fewer communication links and/or where medical and scientific infrastructure is often less developed [ 11 ].
FOSH approaches to support global health systems In recent years, scientists, engineers, and hobbyists have increasingly joined forces to develop and test an impressive array of open source and advanced tools that relate in some way to modern biology, medicine, and aspects of disaster response (e.g. [ 12 – 23 ]). For example, following the 2011 Fukushima nuclear disaster, Safecast [ 9 ] developed the FOSH Geiger counter along with an open-access logging system to map large-scale nuclear contamination in the region driven by citizen science [ 9 ]. Now, the same team is stepping up to meet the challenges of COVID-19 [ 24 ]. Other community-driven FOSH designs relevant to the current situation include simple tools such as DIY masks [25, 26] or 3D-printed valves for regulating airflow in ventilator tubes [27], as well as state-of-the-art scientific instruments for diagnostics , such as automatic pipetting robots [28], microplate readers [29], and various medical tools and supplies [22]. Various further initiatives are well underway, including numerous designs for FOSH ventilators [ 30 – 38 ]. Here, we provide a brief overview of the latest developments in currently available designs and ongoing community projects that aim to leverage FOSH to meaningfully contribute to the global response to the current crisis (see also Box 1). In the specific context of COVID-19, we highlight a set of available projects, centered around:
Personal protective equipment (PPE) such as masks and goggles Patient treatment, focus on ventilators Diagnostic tools, focus on scientific equipment and test kits
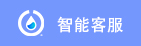
Construction Personal Protective Equipment (PPE) Now that it is becoming increasingly difficult to purchase off-the-shelf masks, people are naturally looking for DIY options that can serve as useful alternatives. Likewise, hospitals are running out of personal protective equipment (PPE) for medical staff, which often includes masks and goggles, as well as specialized clothing and gloves. Here, we will focus on DIY masks and goggles (Figure 1, Table 1).
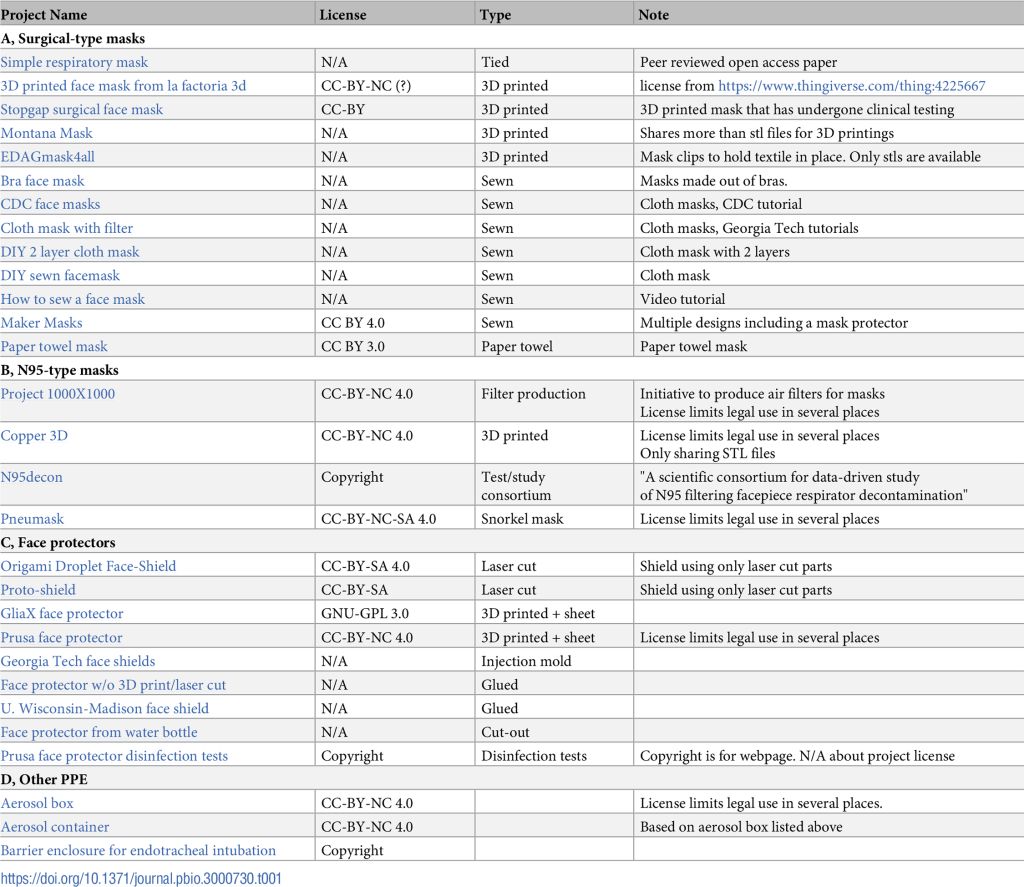
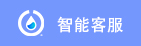
First, it is important to consider what level of protection is required. For example, there are many types of masks with different uses and regulatory standards [ 48-51 ]. Some simpler masks, often called surgical masks, are used by infected people to reduce the spread of infection by catching large droplets, such as after coughing and sneezing. Such masks are easy to make at home (e.g. [ 52 ], Table 1A), but they are generally not considered an effective way to prevent infection [ 21 , 22 , 35 ]. Nonetheless, it has been suggested that they can reduce the spread of viral particles from infected individuals [53]. This was elaborated on in a recent influential paper [ 54 ], but this study did not study SARS-CoV-2, nor possible transmission by asymptomatic carriers (see also [ 55 ]). Another study of four COVID-19 patients found that medical masks were ineffective in preventing the spread of SARS-CoV2 [ 56 ]. Whether medical masks should be recommended for public use, and in what specific circumstances, remains a matter of ongoing debate. At the time of writing, the World Health Organization (WHO) recommends:
If you are healthy, you only need to wear a mask when caring for someone with suspected 2019-nCoV infection. If you cough or sneeze, wear a mask. For an up-to-date summary of the effects and uses of various masks, see their official recommendations [ 57 ]. Of note, the US Centers for Disease Control (CDC) currently recommends wearing masks in public settings where other social distancing measures are difficult to maintain, especially in areas with significant community transmission [ 58 ]. Additionally, other countries are likely to follow suit, especially as the world reopens.
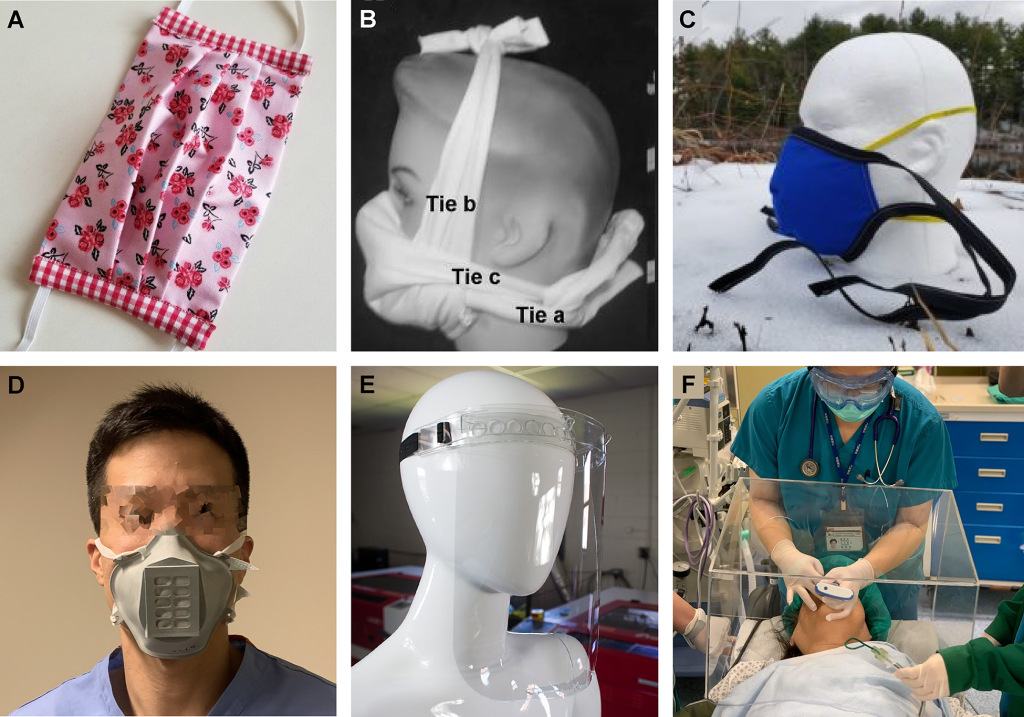
Unlike medical masks, so-called N95 filtering facepiece respirators (FFR) are designed to provide a high level of protection to the wearer, such as would be used by medical staff when caring for infected patients, for example. Unlike medical masks, these masks are designed to seal to prevent air from escaping through the gap between the skin and the mask, and contain specialized filters within the mask that act as a physical barrier to block particles as small as 0.3 microns. This is still larger than an actual virus (about 0.12 microns) [ 59 ], but much smaller than most droplets expelled when sneezing or coughing. The performance standards for such masks are strictly regulated [ 48 - 51 ] and any DIY approach to replicating these masks must carefully refer to these regulations, which may also vary from location to location. Therefore, controlled testing of existing and upcoming N95-type FFR prototypes is critical. Furthermore, if worn incorrectly, they may end up being of little use as medical masks [ 57 ]. For eye protection, N95s can be used in conjunction with tight-fitting goggles or a face shield.
Currently, there are many different types of mask DIY designs on the market, ranging from simple video tutorials based on napkins, cloth, or bra cups (Table 1A) [60-62], to 3D printing options [63], to peer-reviewed scientific studies Designs developed and/or tested [25, 26] (Fig. 1). Some designs are very effective [ 25 ], but to our knowledge, none have fully met regulatory standards to date. However, with designs currently being released on a daily basis, that may soon change. Table 1B summarizes the subset of DIY N95 projects available at the time of this writing.
Alternatively, medical personnel can use splash-resistant surgical masks (IIR, resistant to 160 mmHg) and face shields [ 42 ]. The latter combination may be easier to meet regulatory standards than N95 masks [ 56 ], in part because they do not need to fit tightly against the skin. An online search quickly turns up several designs of masks (and IIR [44]) with varying levels of associated testing [64,65] (Table 1C, Figure 1E). For example, 3D Crowd is a UK-based citizen network that is mobilizing volunteers to produce DIY face coverings to deliver to hospitals and healthcare facilities [ 66 ]. Through “The Big Print,” they have collected requests for 370,000 units. More than 5,500 volunteers are currently producing 80,000 of them. Another approach is based on existing full-face snorkel masks [ 67 ], which can be effectively used as a combination mask and goggles. Efforts such as this, including their important experimental validation, can be easily scaled up with minimal investment. They may also be easier to disinfect for reuse than masks [ 68 , 69 ].
In addition, more specialized personal protective equipment is also actively being developed. This includes DIY testing chambers for diagnostics (requiring virus inactivation in a biosafety level 2 facility BSL2 prior to testing, see below) and DIY aerosol cartridges, for example for intubating patients (Figure 1F, Table 1D) . As with all medical devices, these require regulatory approval [ 48 – 51 ].
The selection of construction materials for PPE should take careful consideration of the construction materials. For example, it has been suggested that the porosity of 3D printing materials may make them a dangerous choice for making masks, as they may allow viral droplets to persist for extended periods of time [ 68 ]. Gaps that may exist in the material itself (e.g. due to bubbling or imperfect delamination during the printing process) further add to the scope for concern. At the time of writing, we are not aware of the available data on the above points. Likewise, when laser cutting parts, the need to use acrylics should be carefully weighed against the need to sterilize them with alcohol or peroxide, which can react with acrylics. If available, and if a laser cutter on hand can handle it (many cannot), polycarbonate or polyethylene terephthalate glycol (PETG) sheets may be a safer choice. DIY PPE disinfection guidance can be found here [ 70 ]. Throughout the process, it is also important to consider possible changes in quality due to the building process itself.
FOSH Ventilator A ventilator is a medical device that supports or takes over a patient's breathing by delivering air or other mixed gases. Patients who are able to breathe on their own are usually treated with constant airflow from an intubation or positive pressure mask (PPM). In more severe cases, the patient may need to be intubated (a tube inserted into the patient's airway). In this case, some modern ventilators can synchronize the release of gas with any remaining attempts at natural breathing. In other cases, the ventilator can take over completely (often in conjunction with patient sedation). At the end of treatment, the patient must be carefully weaned from the ventilator. In general, using a ventilator carries risks of infection, including pneumonia, lung damage, and oxygen toxicity. The latter two may sometimes be related to improper use of equipment (e.g. too high air pressure and/or too high oxygen concentration).
From a technical perspective, a ventilator can be as simple as a manually operated compression bag (Bag Mask - BVM) or as complex as a fully computerized machine that regulates gas pressure, humidity, relative gas concentration, and circulation rate while performing real-time Measurements are taken to monitor patient condition. Some more modern systems add to this complexity, making them more suitable for long-term use because they better simulate physiological conditions and can be adjusted to the patient's specific needs. The National Institutes of Health (NIH) provides an overview of ventilators and their use [ 71 ], including various interface types, ventilator features, and other details not covered in this article. The UK has also recently published its own specifications for hospital ventilators [ 72 ].
The use of non-invasive respiratory systems for COVID-19 patients is currently controversial in hospitals because such systems may generate aerosols that increase the risk of infecting others [ 73 ]. Nonetheless, some believe that non-invasive respiratory systems can be useful in certain circumstances [ 74 ], and the use of such systems may increase as conditions worsen. However, only invasive respiratory systems can completely take over breathing when necessary.
Today, ventilators are already limited for patient care, and this situation may become more severe in the near future [75–77]. Current efforts to resolve this impasse include halting elective surgeries to free up existing systems [78], reactivating deprecated models in warehouses, and calling on industry to increase production [1, 79]. At the same time, diverse groups around the world are convening their communities to design FOSH solutions to help increase ventilator availability (Figure 2, Table 2). Some examples include the development of complete and self-contained systems [ 80 , 81 ], automation of manual ventilators [ 31 , 33 , 37 ], and repair of existing but decommissioned equipment, such as using 3D printed replacement parts [ 82 , 83 ]. Many projects are actively looking for collaborators with diverse backgrounds. FOSH ventilators for invasive use require the implementation of sensor-based feedback systems to measure pressure, carbon dioxide and oxygen levels, tidal volume and dead space volume, and air humidity. These are necessary measurements to know if the machine is performing as expected and not causing further harm to the patient.
The experienced service team and strong production support team provide customers with worry-free order services.

简体中文

繁體中文

English

日本語

한국인